Searching for bacteria that protect against IBD
by Lindzi Wessel
CMIT researchers are pinpointing bacterial species that trigger the development of special immune cells which may be protective against ulcerative colitis and other inflammatory disorders.
Our immune systems are charged with identifying dangerous invaders and taking them out before they can cause serious harm. Sometimes, though, the immune system overdoes it, responding by mistake to things that are harmless—or even sometimes helpful—in a process that leaves our own cells and tissues as collateral damage. This kind of immune overreaction is responsible for a variety of diseases including Crohn’s disease and ulcerative colitis.
Now, CMIT researchers have identified a bacterial signal that promotes the development of special immune cells that might help prevent such immune disorders. The presence of this molecular signal, common to many microbes of the gut, reduced the severity of symptoms in a colitis mouse model, the researchers reported in a summer issue of Science. Understanding how these gut microbes interact with the immune system could eventually help researchers determine how to treat similar human inflammatory bowel diseases, which affect more than three million people in the United States and millions more worldwide.
“This paper gives us a concrete example of how microbes in the gut can orchestrate immunity,” says Hidde Ploegh, one of the paper’s senior authors, a CMIT microbiologist and Professor of Cellular and Molecular Medicine at Boston Children’s Hospital. “Understanding more about how this works is going to help us understand why some people get immune disorders when others don’t and what, ultimately, we can do about it.”
Patrolling gone awry
All along the length of your digestive tract subsists a vibrant and bustling ecosystem made up of hundreds of different kinds of cells—some are yours and some are the bacteria of other tiny lifeforms that together constitute your gut microbiome. Like the plants and critters that might take up residence on the surface of a riverbed, these microbes benefit from nutrients and water that flow down the digestive tract in the form of our food and beverages. And just as the overall health of a river depends on delicate balances that exist among the species that use it, a delicate interplay between the microbes of your gut is critical for the overall health of your digestive tract. Our immune systems, thus, need to be able to recognize “good” microbes and leave them alone, while still remaining vigilant in the face of dangerous pathogens.
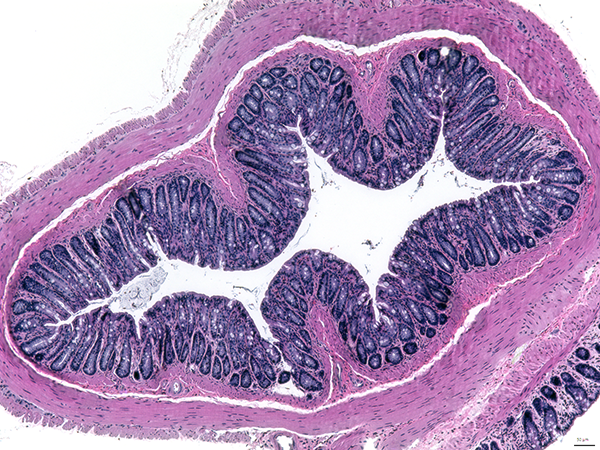
Just how that happens, though, remains an open question. Researchers have long been trying to understand how immune cells make such distinctions and execute a proper response. What we do know, however, is that the result of a false alarm or overreaction can be devastating. Unlike a riverbed, the surface of our intestines is alive and composed of layers of cells responsible for moving food along and absorbing fluids and nutrients, among other functions. When our immune system wages war over this delicate terrain, we wind up injured. In ulcerative colitis and other inflammatory bowel diseases, out of control immune battles can leave patients with inflammation, bleeding and sores in their intestines, which, in turn, drive pain and diarrhea and disrupt the proper absorption of nutrients from food.
“Inflammatory bowel diseases like colitis can be debilitating and difficult to treat,” says Eric Alm, Co-Director of CMIT, Professor of Biological Engineering at MIT, and one of the paper’s senior authors. “More and more evidence suggests the health of our microbiomes are involved, but we’ve yet to map out the concrete relationships between individual microbial species and specific immune cell types that are likely contributing.”
A biochemical tour de force
To understand how bacteria of the digestive system might affect immunity, CMIT researchers chose to examine an important subset of gut immune cells called CD4IELs. Along with another subset of lymphocytes, called regulatory T cells, CD4IELs function as upper management within the intestinal immune system, helping to both raise the alarm in the face of dangerous invaders and to tamp down unnecessary attacks when everything is safe. Despite their importance to basic immune function, recent research has found that these critical cells don’t develop on their own—they can only develop in the presence of intestinal microbiota. Indeed, in mice given antibiotics, which kill gut bacteria, CD4IELs also decline. But due to the challenge of isolating CD4IELs from more populous immune cells of the gut, these lymphocytes are notoriously understudied, and exactly which bacteria drive them to emerge has remained a mystery.
But CMIT researchers are on the case. Taking advantage of a genetically engineered mouse designed to produce only one kind of lymphocyte, which was able to give rise to CD4IELs, the scientists began to isolate species of bacteria from fecal samples, testing one after another to see if any could cause these lymphocytes to turn into CD4IELs. Finally after hundreds of tests, they found a match. In the presence of a common gut bacteria called P. goldsteinii, lymphocytes from the engineered mouse turned into CD4IELs. The researchers didn’t stop there, however. Using cutting-edge technology, the team cut P. goldsteinii bacteria into pieces, hoping to find the exact bacterial protein that could be sprinkled onto their lymphocytes in order to turn them into CD4IELs. Dozens more tests yielded an answer: a protein thought to be important in breaking down sugars, dubbed β-hex, was responsible for the transformation.
“This was a true biochemical tour-de-force and the study’s first author deserves a ton of credit,” says Ploegh, referring to CMIT member and MIT microbiology graduate student Djenet Bousbaine. “The information she found now means we can interrogate any database of microbes to get a list of bacteria that have β-hex as a protein, and thus, may play a role in CD4IEL formation.”
But Bousbaine did not stop there. She and her team had noticed that not all bacteria sporting β-hex could turn their lymphocytes into CD4IELs, likely, she thought, because the β-hex protein could come in different forms. She thus continued her experiments until she identified the exact amino acid sequence that did the trick and then used that information to list known gut bacteria that would likely have the same function.
“What I find extraordinary is that although we’re looking at just one kind of T lymphocyte, we found that a broad set of microbes, which belong to the most abundant phylum found in the mammalian intestines, can induce the development of CD4IELs,” says Angelina Bilate, a CMIT collaborator and Research Associate in Mucosal Immunity at Rockefeller University. “That could have important implications for future therapies involving bacteria.”
A hope for therapy
Indeed, the next step was to test their findings in a mouse model of colitis. Could the bacteria they’d pinpointed have a positive impact in mice sick with a disease akin to colitis? Could β-hex by itself? The answer was yes. Not only did CD4IELs form under these conditions, but half the mice showed improvements in their symptoms. Sick mice with β-hex-induced CD4IELs were less likely to suffer extreme weight loss and showed lower levels of intestinal inflammation compared to sick mice without.
Many treatments for severe forms of colitis and other IBDs rely on drugs that cut inflammation and, in some cases, suppress the immune system. In the worst cases, patients might have no choice but to undergo surgery to remove significant portions of their intestines. Researchers hope, however, that a better understanding of how a healthy gut microbiome leads to a healthy gut immune system will lead to much less invasive future therapies.
“In most people we don’t see immune diseases—our immune system learns how to distinguish friends — cells from our own body and components from our food and helpful bacteria — from foe such as harmful pathogens.’” says Bousbaine. “However, we have limited understanding of how beneficial microbes communicate with our immune system and if we could start to identify some of the signals involved, like we have here, that’s a huge step in the right direction.”

